Autism spectrum disorders comprise a diverse group of conditions involving developmental problems of the nervous system, which affect the interactions with the environment and other people. They are characterized by social and communication difficulties, repetitive behaviors, and unusual sensory responses.
The World Health Organization estimates that about one in 160 children has one of these disorders worldwide. The scientific evidence suggests many factors can make a child more sensitive to developing this pathology, including environmental and genetic factors.
Gut disorders and autism
A substantial amount of research showed that disruptions in the original bacterial composition of the gut, known as dysbiosis, can increase the prevalence of digestive problems, allergies, autoimmune diseases, and psychiatric problems like depression. In the last fifteen years, an increasing number of publications have revealed differences in the composition of gut bacteria in people diagnosed with autism. These studies have boosted the interest in the potential contribution of these communities to autism spectrum disorder.
The egg or the chicken?
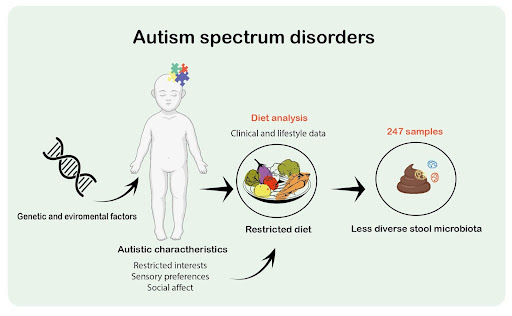
Despite all the work done linking gut dysbiosis with the development of autism, new research showed that we should not blame yet the microbiota for this disease. In a recent study published in Cell, Yap and Gratten from The University of Queensland in Australia tested the hypothesis that the imbalance in gut microbiota caused autism spectrum disorders.
They analyzed stool samples from 247 children aged 2-17, including 99 with autism, 51 siblings not diagnosed with autism, and 97 unrelated children without an autism diagnosis as control groups.
Yap and colleagues extensively characterized the stool samples to identify the different bacteria species and registered the diet of each kid. Surprisingly, researchers found a high relationship between the type of diet of the child and the diversity of the microbiota. Children diagnosed with autism presented a less complex community of bacteria because of a less diverse diet. Yap explained that this could reflect behavioral characteristics: children with autism have a restrictive food selection, often because of allergies concerns.
Compared to other published research, in this study, scientists didn’t find an association between the bacteria stool variation and autism diagnosis; instead, they found it was highly related to diet and age. Only one bacteria (Romboutsia timonensis) appears mostly in the stools of kids with autism. These results suggest an alternative explanation where autism-related characteristics like repetitive behaviors, social skill problems, and sensory sensitivity promote a less diverse diet, consequently less diverse gut microbiota.
Nowadays, more and more research is devoted to finding alternative treatments for neurological disorders like autism. The gut-brain axis and the microbiome emerge as potential targets; yet, Yap and colleagues advise that causality should be addressed carefully to avoid bias. Despite this intense concern and the recent progression of fecal microbiota transplantation as a treatment for autism, the contribution of gut bacteria to these disorders is still inconclusive.
References
Autism spectrum disorders. (2021, June 1). World Health Organization.
Yap, C. X., Henders, A. K., Alvares, G. A., Wood, D. L., Krause, L., Tyson, G. W., Restuadi, R., Wallace, L., McLaren, T., Hansell, N. K., Cleary, D., Grove, R., Hafekost, C., Harun, A., Holdsworth, H., Jellett, R., Khan, F., Lawson, L. P., Leslie, J., . . . Gratten, J. (2021). Autism-related dietary preferences mediate autism-gut microbiome associations. Cell, 184(24), 5916–5931.e17. https://doi.org/10.1016/j.cell.2021.10.015
Hodges, H., Fealko, C., & Soares, N. (2020). Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation. Translational Pediatrics, 9(S1), S55–S65. https://doi.org/10.21037/tp.2019.09.09
Featured illustration: Sofía Polcowñuk.





